Condition
Pediatric Cloacal Malformations
What You Need to Know
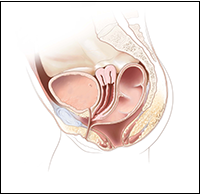
A cloacal malformation, which occurs in a female fetus, is when the rectum, vagina and urinary tract form a single channel known as a cloaca, rather than three separate openings.
Key Symptoms
Patients with cloacal malformation may have symptoms such as:
- Abdominal swelling
- Kidney issues
- Fluid backup into the vagina and uterus
Diagnosis
The following diagnostic tests may be used to evaluate newborns with cloacal malformations:
- Abdominal ultrasound
- Spinal ultrasound
- X-rays
Treatment
As part of long-term follow up care, treatment may include:
- Cloacal malformation reconstructive surgery
- Catheterization of the urinary system to ensure good emptying of the bladder
- Participation in a bowel management program
What Are Pediatric Cloacal Malformations?
A cloacal malformation is a type of anorectal malformation that occurs in a female fetus when the rectum, vagina and urinary tract form a single channel known as a cloaca rather than three separate openings. The severity of the condition depends on where the three tracts have joined together. Cloacal malformations occur when the embryonic anorectal and urogenital channels fail to separate during the sixth and seventh weeks of gestational development. This condition is rare; cloacal malformations only occur in approximately 1 in 50,000 live births.
Cloacal Exstrophy
Cloacal exstrophy is one of the most complicated and severe forms of cloacal malformations. It occurs when a baby is born with several organs that are exposed, such as the bladder or large intestine, and is combined often with these organs protruding from the navel (called an omphalocele).
Common Types of Cloaca
Cloaca with a short common channel
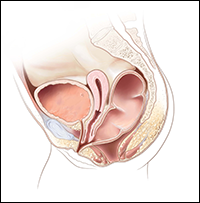
Cloaca with a long common channel
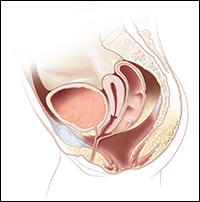
Cloaca with a very high rectum
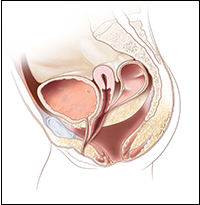
Cloaca with two hydrocolpos
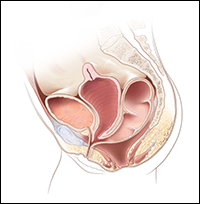
Cloaca with two hemivaginas
Recognizing Cloacal Malformation Symptoms
Newborn babies with cloacal malformations do not have visible anuses. Urine usually successfully passes, but it is mixed with vaginal mucous and stool. They also may have symptoms or complications such as:
- Abdominal swelling
- Enlarged kidneys
- Having only one kidney
- Hydrocolpos — a condition causing fluid to back up in the vagina and uterus, which can cause a blockage of the ureters
- Urine that backs up into the kidneys (reflux)
- Problems with function of gynecologic organs that may persist into adulthood
Prenatal testing sometimes detects cloacal malformations before birth. Early treatment is required to lessen complications.
Diagnosis of Cloacal Malformation in Infants at Children's National
In some cases, doctors may be able to diagnose the malformation in utero. However, in most cases, making an accurate diagnosis requires a physical examination and various diagnostic tests after the baby is born. Children's National expert pediatric colorectal surgeons, urologists and gynecologists use the latest diagnostic tests and tools to evaluate for all the possible defects that could be related to your child’s condition.
When evaluating a newborn with a suspected cloacal malformation, the following diagnostic tests may be used:
- Abdominal ultrasound. To examine the kidneys, bladder, gynecologic system and pelvic organs
- Spinal ultrasound. To evaluate for spine abnormalities or other neurological problems such as tethered cord or myelomeningocele
- X-rays. To examine the spine and sacrum
Imaging tests are very important because children diagnosed with this condition may also have anomalies in other organ systems.
3D Cloacagram
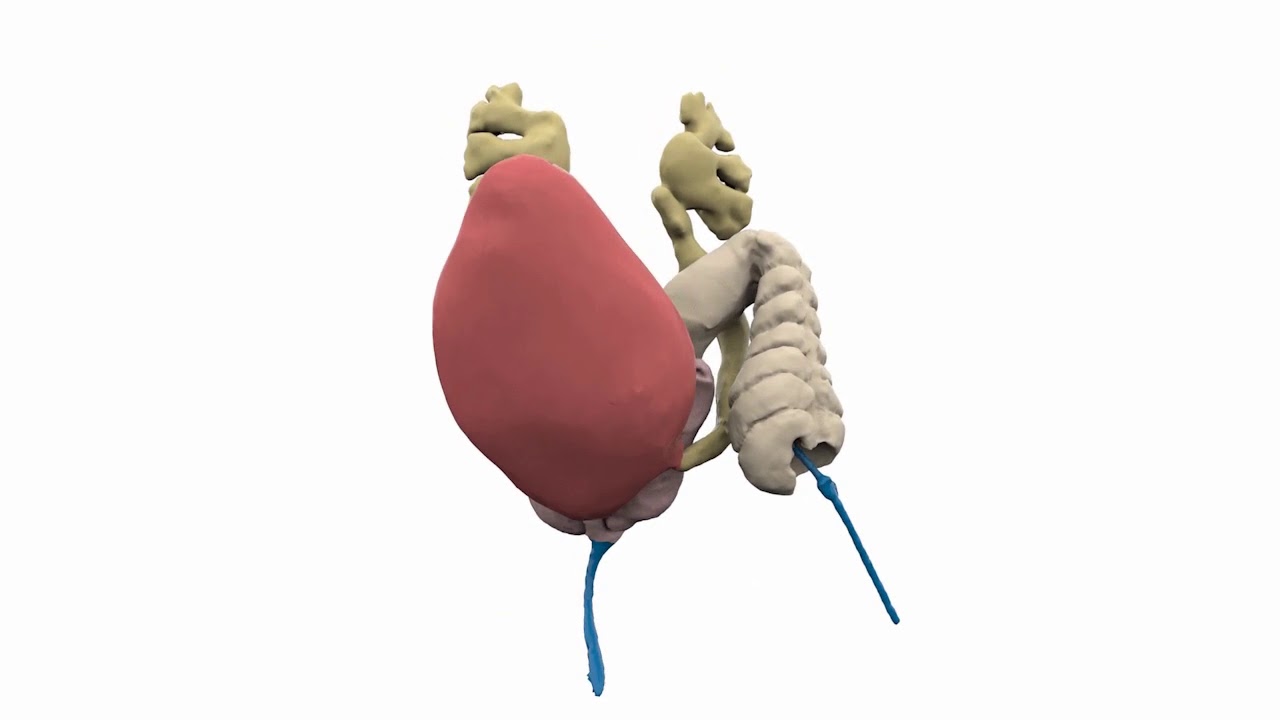
A pediatric team may also use a 3D cloacagram, as seen in this video, to help define the anatomy detected on the imaging and plan for surgery. A cloacagram can be helpful in detecting the type of cloaca that is present.
Treatment Approaches for Pediatric Cloacal Malformations
Cloacal malformations can be very complex and require multidisciplinary treatment from several different specialists.
- Birth and stabilization. Immediate treatment of the newborn will entail drainage of the urine and a colostomy to allow stool to exit the body. Once the baby has stabilized, a comprehensive diagnosis will be completed.
- Imaging and diagnosis. The medical team may order an abdominal and pelvic ultrasound to obtain high-definition images of the spine and pelvis. An endoscopic examination, taking place after the neonatal period, may also be recommended as it allows the team to obtain a more detailed anatomical understanding of the malformation.
- Treatment plan. Based on the radiologic testing and examination results, the medical team will create an individualized treatment plan unique to your baby’s specific condition that will involve surgical reconstruction. This involves collaboration of the colorectal, urologic and gynecologic teams at all stages of care.
- Surgery. Reconstructive surgery often includes constructing or correcting channels to separate the urethra and vagina functions. Pull-through surgery may be required to re-attach the colon to the anus. Additional surgery will likely be needed to close the ostomy that was created at birth.
- Catheterization. Sometimes, patients need catheterization to drain their bladder. This is when a thin, flexible tube is inserted through the urethra and into the bladder to remove urine.
The Pediatric Colorectal & Pelvic Reconstruction Program team at Children's National Hospital has the world's greatest volume of experience in surgically treating cloacas, and in particular the most complex types of cloacal malformations, and specializes in the repair of colorectal, urologic and gynecologic organs.
Helping Your Child Recover from Surgery
Recovery from cloacal malformation reconstructive surgery will typically require several or more days in the hospital. Your child will need to be closely supervised to make sure the urethra, vagina and rectum have adequately healed.
As with all anorectal malformations, surgery will restore some function, but the nerves and muscles that control the bowels may still be weak. Children who have had surgery for anorectal malformations may experience fecal incontinence or constipation, but this can be well managed using our bowel management program.
For patients who need it, the bowel management program can help facilitate optimal bowel function in combination with following a healthy diet rich in fiber to combat constipation. Children’s National’s bowel management program consists of a week-long outpatient program followed by ongoing appointments (as needed) until the child can remain clean and dry. The program is individualized based on the patient’s diagnosis, age, symptoms, medical history and goals. It’s offered 12 to 15 times per year.
Some patients require continued catheterization of the urinary system to ensure good emptying of the bladder. All patients require long-term monitoring of kidney function. Your medical team will discuss what recovery will entail for your child.
Long-Term Care for Infant Cloacal Malformations
Children born with cloacal malformations require long-term, continued follow-up care as this condition can increase the risk of certain urological, gynecological and colorectal conditions.
During Childhood
Entering Adolescence
Learn More in Our Educational Videos
Our Pediatric Colorectal and Pelvic Reconstruction team has produced a series of educational videos on topics such as care following a pull-through procedure for a child with Hirschsprung's disease and much more. We hope that families facing colorectal conditions can better navigate their care journey by watching the videos.
About Cloacal Malformations
Children with cloacal malformations require long-term, continued care as they are at increased risk of developing certain urological, gynecological and colorectal conditions later in life. Learn about treatment, post-operative issues and long-term outcomes.
Schedule an Appointment
At Children's National, our providers are some of the most renowned and experienced pediatric colorectal specialists in the world. Plus, we offer colorectal care for life, making transitions into adolescence and adulthood healthier. Book your child's appointment today.
Ariana Charts Her Own Path
Successful surgeries and expert guidance about her rare congenital condition gave Ariana the ability, independence and courage to thrive.
Departments that Treat Cloacal Malformations

Pediatric Colorectal & Pelvic Reconstruction
The Division of Pediatric Colorectal & Pelvic Reconstruction offers the latest advancements in diagnosis and treatment for all types of pediatric colorectal disorders. Learn more about our division.