Treatment
Kidney Transplantation
Key Points about Kidney Transplants in Children
- A kidney transplant is surgery to place a healthy kidney from another person into someone with severe kidney problems.
- Transplanted organs can come from deceased or living donors — and you could be a match.
- You and your child will work with a comprehensive kidney transplant team before, during and after the process which will include evaluations, diagnostic tests and a period of waiting for the right match.
- Living with a transplant is a lifelong process. Antirejection medicine (immunosuppressants) must be taken for the rest of your child’s life.
Frequently Asked Questions
About Kidney Transplants
What is a kidney transplant?
A kidney transplant is surgery to place a healthy kidney from another person into someone with severe kidney problems. The healthy kidney may come from two types of donors:
- Deceased donor. This is an organ donor who has just died
- Living donor. Family members or people who are unrelated but make a good match may be able to donate one of their kidneys. This is called a living transplant. People who donate a kidney can live healthy lives with their one remaining kidney.
A child receiving a transplant usually receives only one kidney. But in rare cases a child may receive two kidneys from a deceased donor. In most cases, the diseased kidneys are left in place during the surgery. The transplanted kidney is placed in the lower belly (abdomen) on the front side of the body.
Why is a kidney transplant recommended?
A kidney transplant is recommended for children who have serious kidney problems and will die without dialysis or a transplant. Some of the kidney diseases in children that may require a transplant include the following:
- Birth defects and heredity diseases. These are the most common causes of kidney failure in children from birth to age 4
- Heredity diseases, nephrotic syndrome and systemic diseases. These are the most common cause of kidney failure in children between ages 5 and 15
- Diseases that affect the blood vessels (glomeruli) in the kidneys. The most common cause of kidney failure in children between ages 15 and 19
Not all children with these diseases will need a kidney transplant. Always see your child's healthcare provider for a diagnosis.
Where do transplanted organs come from?
There are two types of donors: deceased donors and living donors.
Deceased Donors
Most transplanted kidneys come from deceased organ donors. This is called a deceased donor transplant. These organ donors are adults or children who have become critically ill and are pronounced dead because their brain or their heart has stopped working. If the donor is an adult, he or she may have agreed to be an organ donor before becoming ill. The family of the deceased person must agree to donate the person's organs. Donors can come from any part of the United States. A child receiving a transplant usually receives only one kidney, but in rare cases a child may receive two kidneys from a deceased donor. Researchers are also experimenting with splitting one kidney for two recipients.
Living Donors
Family members or people who are not related but are a good match may also be able to donate one of their kidneys. This is called a living transplant. People who donate a kidney can live healthy lives with the one kidney that remains. A child over age 2 can generally receive an adult kidney. There is usually enough space in the child’s belly for the new kidney to fit.
Waiting for a Kidney Transplant
What is the transplant waiting list?
If your child is accepted as a transplant candidate, he or she will be placed on a national transplant waiting list. When a donor organ becomes available, a computer searches all the people on the waiting list for a kidney. Those who are not good matches for the available kidney are set aside. A new list is made from the remaining candidates.
The person at the top of the specialized list is considered for the transplant. If he or she is not a good candidate, for whatever reason, then the next person is considered. In some cases, people lower on the list may be considered before a person at the top. This can happen for different reasons. These include the donor organ’s size or how far away the donor is from the recipient.
How is my child placed on the waiting list for a new kidney?
Talk with your child’s healthcare team to see if a transplant is an option for your child. If it is, then have your child’s provider refer you to a transplant center in your area. Transplant centers are located in certain hospitals throughout the U.S. Your child must complete a full evaluation at the transplant center.
Your child will have a variety of tests done by the transplant center team. This is the group of specialists who evaluate people to see if they can have a transplant procedure. They also care for people undergoing a transplant. The team will decide if your child is a candidate for a transplant.
The transplant center team will include:
- Transplant surgeons. Doctors who specialize in transplantation and who will be performing the surgery. The transplant surgeons coordinate all team members. They follow your child before the transplant and continue to follow your child after the transplant and after discharge from the hospital
- Nephrologists. Doctors who specialize in disorders of the kidneys. Nephrologists will help manage your child before and after the surgery
- Urologists. Doctors who specialize in diagnosis and treatment of disorders of the genitourinary tract
- Transplant nurse coordinator. A nurse who organizes all aspects of care provided to your child before and after the transplant. The nurse coordinator will provide patient education and coordinate the diagnostic testing and follow-up care
- Social workers. Professionals who will provide support and guidance to your family as you deal with many issues that may arise, including lodging and transportation, finances and legal issues. They can also help coordinate alternative means for school, so that your child does not fall behind
- Dietitians. Professionals who will help your child meet his or her nutritional needs before and after the transplant. They will work closely with you and your family
- Physical therapists. Professionals who will help your child become strong and independent with movement and endurance after the transplantation
- Chaplaincy services. Chaplains who provide spiritual care and support
- Other team members. Several other team members will evaluate your child before transplantation and provide follow-up care, as needed. These include, but are not limited to, the following:
- Pharmacists
- Anesthesiologists
- Hematologists
- Infectious disease specialists
- Respiratory therapists
- Lab technicians
- Psychologists
- Child life specialists
The Transplant Evaluation Process
An extensive evaluation must be done before your child can be placed on the national transplant waiting list. Testing includes:
- Blood tests
- Diagnostic tests
- Psychological and social evaluation of the child (if old enough) and the family
Tests are done to gather information that will help determine how urgent it is that your child is placed on the transplant list. These tests also ensure your child receives a donor organ that is a good match. Tests include those to analyze your child’s general health, including:
- Heart, lung and kidney function
- Nutritional status
- The presence of infection
Blood Tests
Blood tests will help improve the chances that the donor organ won’t be rejected. These tests may include:
- Blood chemistries. These may include serum creatinine, electrolytes (such as sodium and potassium), cholesterol and liver function tests
- Clotting studies, such as prothrombin time (PT) and partial thromboplastin time (PTT). These tests measure the time it takes for blood to clot
Other blood tests will help improve the chances that the donor organ will not be rejected. They may include:
- Your child's blood type. Each person has a specific blood type: type A+, A-, B+, B-, AB+, AB-, O+, or O-. When receiving a transfusion, the blood received must be a compatible type with your child's own. If not, an allergic reaction will occur. The same allergic reaction will occur if the blood contained within a donor organ enters your child's body during a transplant. Allergic reactions can be avoided by matching the blood types of your child and the donor
- Human leukocyte antigens (HLA) and panel reactive antibody (PRA). These tests help figure out how successful an organ transplant may be. The tests check for antibodies in your child's blood. Antibodies are made by the body's immune system in reaction to a foreign substance, such as a blood transfusion or a virus. Antibodies in the bloodstream will try to attack transplanted organs. Children who receive a transplant will take medicines that decrease this immune response. The higher your child's PRA, the more likely that an organ will be rejected
- Kidney, liver and other vital organ function tests
- Viral studies. These tests determine if your child has antibodies to viruses that may increase the likelihood of rejecting the donor organ, such as cytomegalovirus (CMV). Many other infectious diseases are also tested for, including HIV and hepatitis
Diagnostic Tests
Extensive diagnostic tests are also done. They are needed to understand your child’s complete health status. Other tests may also be done, including the following:
- Kidney ultrasound. For this noninvasive test, a probe (transducer) is passed over the kidney on the outside of the body. The probe creates sound waves that bounce off the kidney. The sound waves transmit a picture of the kidney onto a video screen. This test is used to determine the size and shape of the kidney. It can also see if there is a mass, kidney stone, cyst or other blockage or abnormality
- Kidney biopsy. Tissue samples are removed (with a needle or during surgery) from the kidney and checked under a microscope
- Intravenous pyelogram (IVP). A series of X-rays of the kidney, ureters and bladder. Contrast dye is injected into the vein to find tumors, abnormalities, kidney stones or any blockages, and to assess renal blood flow
Getting on the List
The transplant team will consider all the information gathered from interviews, your child's medical history and the evaluation tests. Based on this information, the team will decide if your child is a transplant candidate. If your child is a candidate, the transplant team will add him or her to the national transplant waiting list. If you have any questions about your child’s place on the list, ask the transplant team.
How long will it take to get a new kidney?
There is no definite answer to this question. If there is a matching and healthy living donor, your child may be able to get a transplant in a few weeks or months. If no living related donor is available, it may take months or years on the waiting list before a suitable donor organ is available. During this time, your child will receive close follow-up care with his or her healthcare providers and the transplant team. Many support groups are also available to help you during this waiting time.
How are we notified when a kidney is available?
Each transplant team has their own specific guidelines for waiting on the transplant list and being notified when a donor organ is available. In most cases, you will receive a phone call that an organ is available. You will be told to come to the hospital immediately so your child can be prepared for the transplant.
Kidney Transplant Surgery
What is involved in kidney transplant surgery?
Once an organ becomes available to your child, you and your child will be immediately called to the hospital. This call can occur at any time. So you should always be prepared to go to the hospital, if needed. Once at the hospital, your child will have some more final blood work and tests to confirm the organ is a match.
Your child will then go to the operating room. The transplant surgery may take several hours. But this will vary greatly depending on each individual case. During the surgery, a member of the transplant team will keep you informed on how the surgery is going.
What does postoperative care for kidney transplant involve?
After the surgery, your child will go to the intensive care unit (ICU) to be watched closely. The length of time your child will spend in the ICU will vary. It will be based on your child's unique condition. After your child is stable, he or she will be sent to the special unit in the hospital that cares for kidney transplant patients. Your child will continue to be watched closely. You will be educated on all aspects of caring for your child during this time. This will include information about medicines, activity, follow-up, diet and any other specific instructions from your child's transplant team.
What is rejection?
Rejection is the body’s normal reaction to foreign tissue. When a new kidney is placed in a person's body, the body sees the transplanted organ as a threat and tries to attack it. The immune system makes antibodies to try to kill the new organ. To help the new kidney survive in your child’s body, your child must take antirejection medicines (immunosuppressants). These medicines weaken the immune system’s response. Your child must take these medicines for the rest of his or her life.
What are the symptoms of rejection?
Most children who have a kidney transplant do not have symptoms. A rejection episode is suspected via routine blood tests. If a child has symptoms, they may include:
- Fever or flu-like illness
- Soreness over the kidney
- Raised blood creatinine level
- High blood pressure
- Decreased urine output
- Weight gain
Your transplant team will tell you who to call right away if any of these symptoms occur.
What is done to prevent rejection?
Your child must take antirejection medicines for the rest of his or her life. Each child may react differently to medicines, and each transplant team has preferences for different medicines. Some of the antirejection medicines most commonly used include the following:
- Cyclosporine
- Tacrolimus
- Azathioprine
- Mycophenolate mofetil
- Prednisone
- Muromonab-CD3
- Lymphocyte immune globulin
New antirejection medicines are always being approved. Your child’s healthcare provider will create a medicine treatment plan that is right for your child. The doses of these medicines may change frequently as your child's response to them changes. Antirejection medicines affect the immune system. So children who receive a transplant will be at higher risk for infections. A balance must be maintained between preventing rejection and making your child very vulnerable to infection. Your child will have blood tests done regularly. These will measure the amount of medicine in your child’s body and make sure your child does not get too much or too little of the medicines. White blood cells are also an important indicator of how much medicine your child needs.
What about infection?
This risk of infection is especially great in the first few months after the transplant. That is because higher doses of antirejection medicines are given during this time. Your child will most likely need to take medicines to prevent other infections from occurring. Some of the infections your child will be especially vulnerable to include oral yeast infection (thrush), herpes and respiratory viruses.
What is the long-term outlook for a child after a kidney transplant?
Living with a transplant is a lifelong process. Medicines must be given that trick the immune system so it won’t attack the transplanted organ. Other medicines must be given to prevent side effects of the antirejection medicines, such as infection. Frequent visits to and contact with the transplant team are essential. It’s very important to know the signs of organ rejection and to look for them each day. When your child is old enough, he or she will need to learn about antirejection medicines. Your child will need to learn what these medicines do and the signs of rejection. Over time your child must be able to care for himself or herself independently.
Every child is unique and every transplant is different. Results keep improving as healthcare providers and scientists learn more about how the body deals with transplanted organs and search for ways to improve the transplant process.
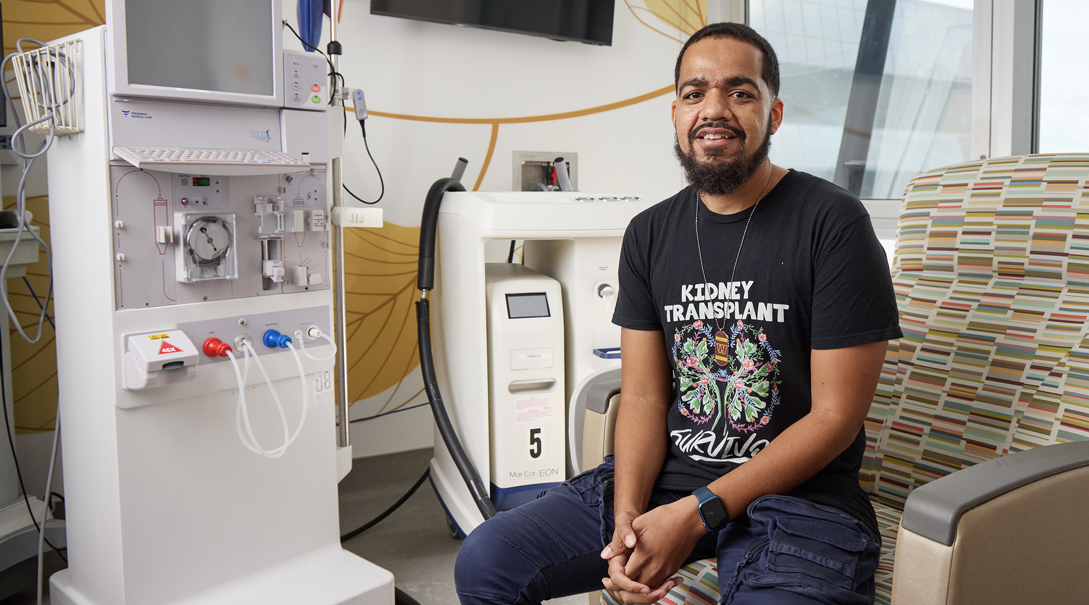
Meet the Kidney Transplantation Providers
Patient Stories
Departments that Offer Kidney Transplantation

Nephrology
Learn how our highly skilled pediatric nephrology team works across divisions to manage the full range of kidney diseases in children, including dialysis and kidney transplantation.

Kidney Transplantation Program
The Kidney Transplantation Program is the only one of its kind in the Washington, D.C., area focused on the needs of children and teens with kidney disease. Additionally, it is the region's only Medicare-approved center for kidney transplants in children and teens.

Bone Health Program
Orthopaedists at Children's National offer world-renowned expertise and life-changing care, including surgery, for children at high risk for bone fracture.

Help Kids and Make a Difference
Invest in future cures for some of life's most devastating diseases. Give today to help more children grow up stronger.