Condition
Pediatric Atrial Septal Defect (ASD)
What You Need to Know
An atrial septal defect (ASD) is an opening in the atrial septum, or dividing wall between the two upper chambers of the heart.
Key Symptoms
The most common symptoms of ASD are:
- Fatigue
- Sweating
- Rapid breathing
- Shortness of breath
- Poor growth
- Frequent respiratory infections
Diagnosis
Doctors typically diagnose ASD by:
- Chest X-ray
- Electrocardiogram (ECG)
- Echocardiogram (echo)
- Cardiac catheterization
Treatment
Treatment for ASD may include:
- Medication
- Surgical repair
- Device closure
Schedule an Appointment
Our pediatric specialists provide personalized care for your child’s physical, mental and emotional health needs. Meet our providers and schedule an appointment today.
Frequently Asked Questions
Prevention and Risk Assessment
What is an atrial septal defect?
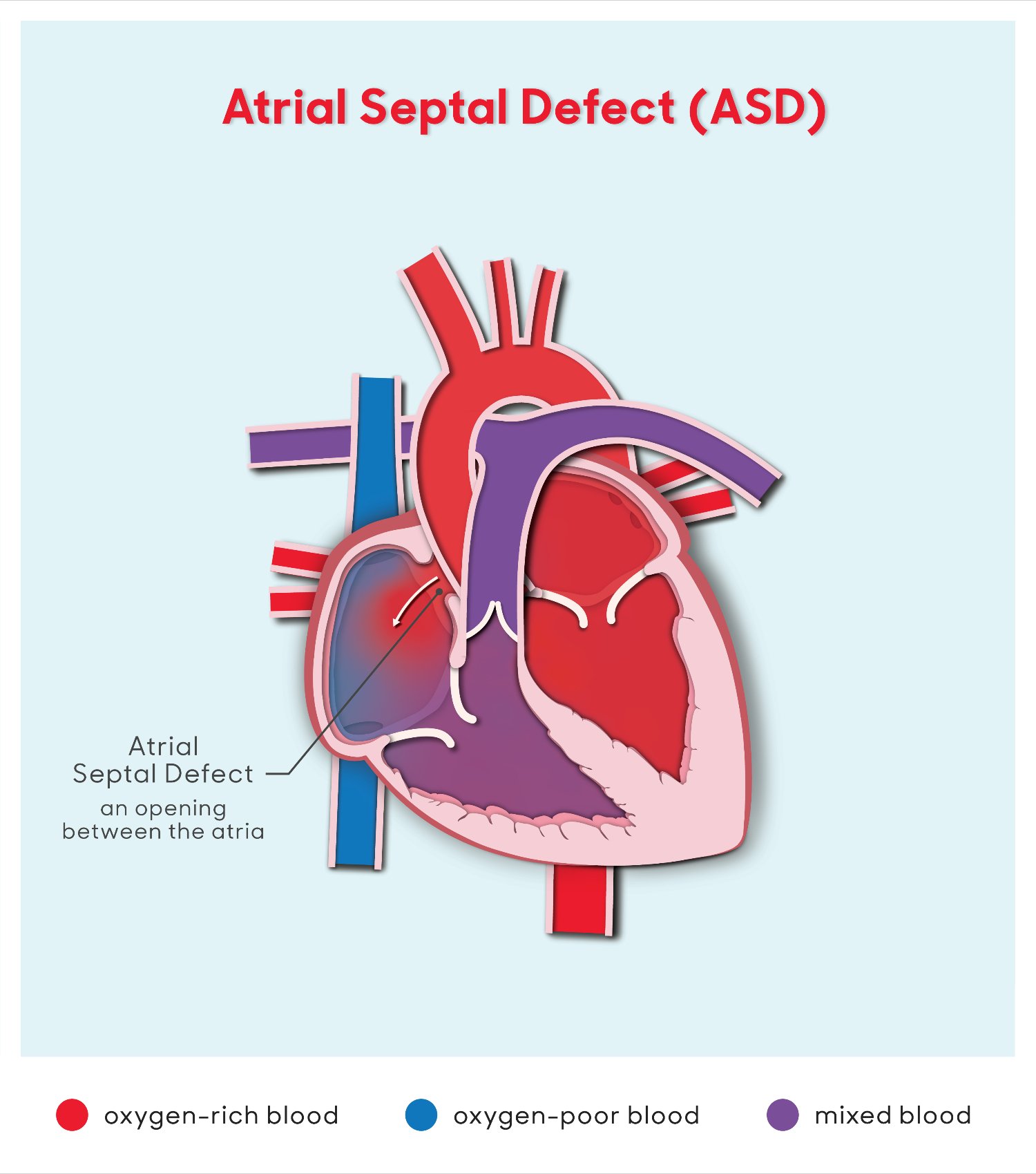
An atrial septal defect is an opening in the atrial septum, or dividing wall between the two upper chambers of the heart, known as the right and left atria. ASD can be a congenital (present at birth) heart defect, or it can result from the failure of normal postnatal closure of a hole that is present in the heart of every fetus.
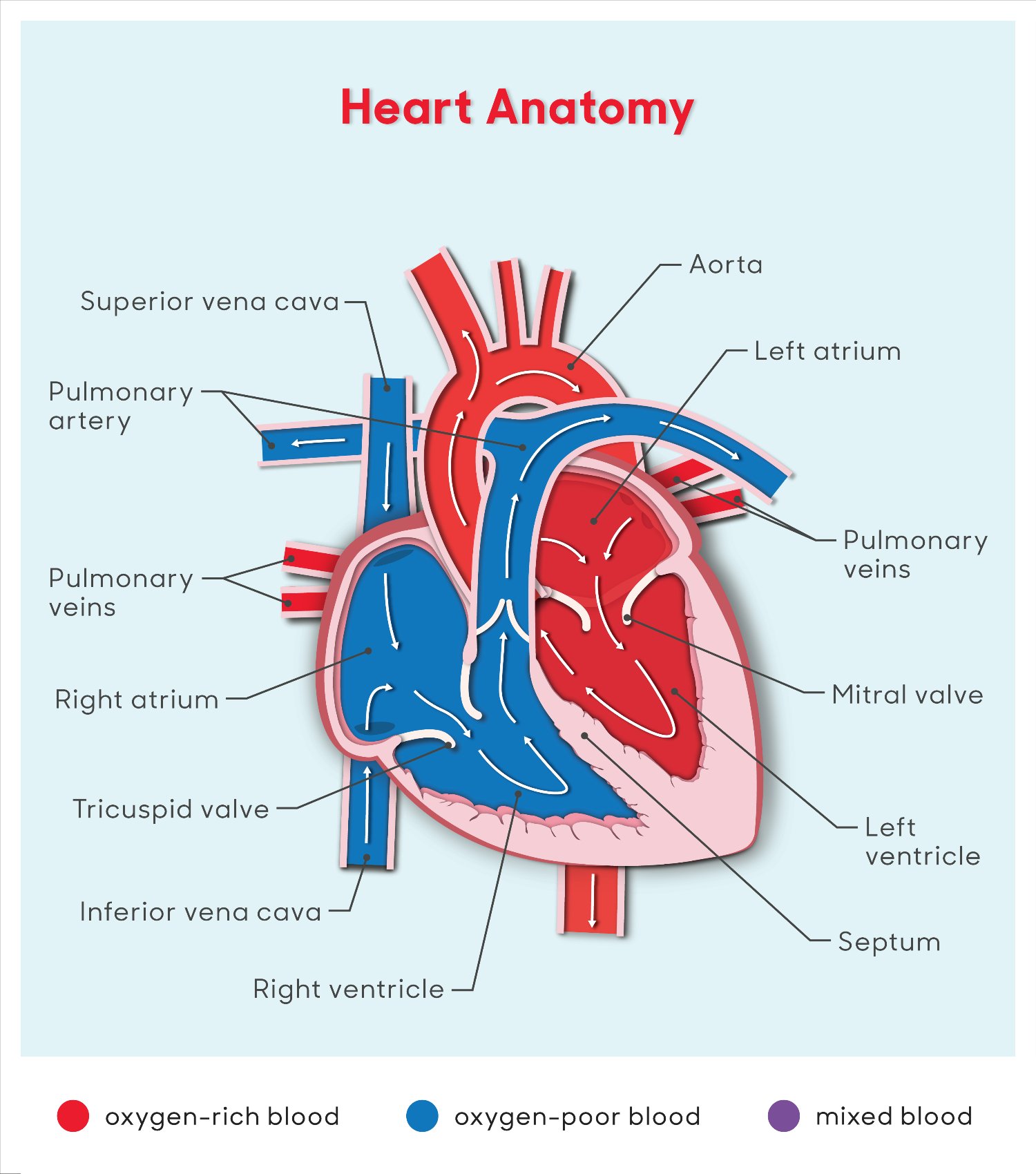
Normally, oxygen-poor (blue) blood returns to the right atrium from the body, travels to the right ventricle, then is pumped into the lungs where it receives oxygen. Oxygen-rich (red) blood returns to the left atrium from the lungs, passes into the left ventricle, and then is pumped out to the body through the aorta.
An atrial septal defect allows oxygen-rich (red) blood to pass from the left atrium, through the opening in the septum, and then mix with oxygen-poor (blue) blood in the right atrium.
 |
Atrial septal defects occur in a small percentage of children born with congenital heart disease. For unknown reasons, girls have atrial septal defects twice as often as boys.
What causes an atrial septal defect in children?
The heart is forming during the first eight weeks of prenatal development. It begins as a hollow tube, then partitions within the tube develop that eventually become the septa (or walls) dividing the right side of the heart from the left. Atrial septal defects usually occur when the partitioning process does not occur completely, leaving an opening in the atrial septum.
Some congenital heart defects may have a genetic link, either occurring due to a defect in a gene, a chromosome abnormality or environmental exposure, causing heart problems to occur more often in certain families. Most atrial septal defects occur sporadically (by chance), with no clear reason for their development.
What are the types of atrial septal defects in children?
There are four major types of atrial septal defects:
- Ostium secundum atrial septal defect. This is the most common atrial septal defect, affecting over two-thirds of people with atrial septal defects. It is caused when a part of the atrial septum fails to close completely while the heart is developing. This causes an opening to develop in the center of the wall separating the two atria.
- Ostium primum atrial septal defect. This defect is part of atrioventricular canal defects and is associated with a split (cleft) in one of the leaflets of the mitral valve.
- Sinus venosus atrial septal defect. This defect occurs at the superior vena cava and right atrium junction in the area where the right pulmonary veins enter the heart. As a result, the drainage of one or more of the pulmonary veins may be abnormal in that the pulmonary veins drain to the right atrium, rather than the left atrium.
- Coronary sinus atrial septal defect. This defect is located within the wall of the coronary sinus, where it passes behind the left atrium. The coronary sinus carries the blood flow from the heart's own vein, into the right atrium. It is the rarest of all atrial septal defects.
Why is an atrial septal defect in children a concern?
This heart defect can over time cause lung problems if not repaired. When blood passes through the ASD from the left atrium to the right atrium, a larger volume of blood than normal must be handled by the right side of the heart. This extra blood passes through the pulmonary artery into the lungs, causing higher amounts of blood flow than normal in the vessels in the lungs.
A small opening in the atrial septum allows a small amount of blood to pass through from the left atrium to the right atrium. A large opening allows more blood to pass through and mix with the normal blood flow in the right heart.
The lungs are able to cope with this extra blood flow for a long period of time. In some patients, the extra blood flow eventually raises the blood pressure in the lungs, usually after several decades. This then hardens the blood vessels in the lungs, causing them to be diseased, resulting in irreversible changes in the lungs.
Diagnosis
What are the symptoms of an atrial septal defect in children?
Many children have no symptoms and seem healthy. However, if the ASD is large, permitting a large amount of blood to pass through to the right side of the heart, the right atrium, right ventricle and lungs will become overworked and symptoms may be noted. The following are the most common symptoms of atrial septal defect. However, each child may experience symptoms differently. Symptoms may include:
- Child tires easily when playing
- Fatigue
- Sweating
- Rapid breathing
- Shortness of breath
- Poor growth
- Frequent respiratory infections
The symptoms of an atrial septal defect may resemble other medical conditions or heart problems. Always consult your child's physician for a diagnosis.
How is an atrial septal defect diagnosed in a child?
Your child's healthcare provider may have heard a heart murmur when listening to your child's heart with a stethoscope. The heart murmur is from the abnormal flow of blood through the heart.
Your child may need to see a pediatric cardiologist for a diagnosis. This is a healthcare provider with special training in treating heart problems in children. This provider will examine your child and listen to your child's heart and lungs. They will find out where the murmur is best heard and how loud it is. Your child may have some tests, such as:
- Chest X-ray. This test may show an enlarged heart. Or it may show changes in your child's lungs because of the blood flow changes caused by an ASD.
- Electrocardiogram (ECG). This test records the electrical activity of the heart. It shows abnormal rhythms (arrhythmias) that may be caused by an ASD. It can also find heart muscle stress caused by an ASD.
- Echocardiogram (echo). This test uses sound waves to make a moving picture of the heart and heart valves. An echo can show the blood flow through the atrial septal opening and find out how big the opening is.
- Cardiac catheterization. This test uses a thin, flexible tube (catheter) put near the heart. Contrast dye is used to get even clearer pictures. In some children, this procedure may be used to close the ASD.
Treatment
What treatment is available for atrial septal defect in children?
Specific treatment for ASD will be determined by your child's physician based on:
- Your child's age, overall health and medical history
- Extent of the disease
- Your child's tolerance for specific medications, procedures or therapies
- Expectations for the course of the disease
- Your opinion or preference
Secundum atrial septal defects may close spontaneously as a child grows. Once an atrial septal defect is diagnosed, your child's cardiologist will evaluate your child periodically to see whether it is closing on its own. Usually, an ASD will be repaired if it has not closed on its own by the time your child starts school — to prevent lung problems that will develop from long-time exposure to extra blood flow. The decision to close the ASD may also depend on the size of the defect. Individuals who have their atrial septal defects repaired in childhood can prevent problems later in life.
Treatment may include:
Medical Management
Many children have no symptoms and require no medications. However, in rare circumstances, children may need to take medications to help their heart work better since the right side is under strain from the extra blood passing through the ASD. Medications may be prescribed, such as diuretics. Diuretics help the kidneys remove excess fluid from the body. This may be necessary because the body's water balance can be affected when the heart is not working as well as it could.
Surgical Repair
Your child's ASD may be repaired surgically in the operating room. The surgical repair is performed under general anesthesia. The defect may be closed with stitches or a special patch.
Device closure
Device closure is frequently performed for secundum ASD, depending on the size of the defect and the weight of the child. During the cardiac catheterization procedure, the child is sedated and a small, thin, flexible tube (catheter) is inserted into a blood vessel in the groin and guided to the inside of the heart. Once the catheter is in the heart, the cardiologist will pass a special device, called a septal occluder, into the open ASD, preventing blood from flowing through it.
Our heart specialists offer expert treatment for ASD closure, including Amplatzer® and Gore® Helex® Septal Occluders.
What should I expect from my child's post-procedure care for an atrial septal defect?
Device Closure Procedure
When the procedure is complete, the catheter(s) will be withdrawn. Several gauze pads and a large piece of medical tape will be placed on the site where the catheter was inserted to prevent bleeding. In some cases, a small, flat weight or sandbag may be used to help keep pressure on the catheterization site and decrease the chance of bleeding. If blood vessels in the leg were used, your child will be told to keep the leg straight for a few hours after the procedure to minimize the chance of bleeding at the catheterization site.
Your child will be taken to a unit in the hospital where he or she will be monitored by nursing staff for several hours after the test. The length of time it takes for your child to wake up after the procedure will depend on the type of medicine given to your child for relaxation prior to the test, and also on your child's reaction to the medication.
After the procedure, your child's nurse will monitor the pulses and skin temperature in the leg or arm that was used for the procedure.
Your child may be able to go home after a specified period of time, providing he or she does not need further treatment or monitoring. You will receive written instructions regarding care of the catheterization site, bathing, activity restrictions and any new medications your child may need to take at home.
Surgical Repair
In most cases, children will spend time in the intensive care unit (ICU) for several hours, or overnight after an ASD repair. During the first several hours after surgery, your child will most likely be drowsy from the anesthesia that was used during the operation and from medications given to relax him or her and to help with pain. As time goes by, your child will become more alert.
While your child is in the ICU, special equipment will be used to help him or her recover and may include the following:
- Ventilator. A machine that helps your child breathe while he or she is under anesthesia during the operation. A small, plastic tube is guided into the windpipe and attached to the ventilator, which breathes for your child while he or she is too sleepy to breathe effectively on his or her own. Many children have the ventilator tube removed right after surgery but some other children will benefit from remaining on the ventilator for a few hours afterwards or overnight so they can rest.
- Intravenous (IV) catheters. Small, plastic tubes inserted through the skin into blood vessels to provide IV fluids and important medications that help your child recover from the operation.
- Arterial line. A specialized IV placed in the wrist or other area of the body where a pulse can be felt that measures blood pressure continuously during surgery and while your child is in the ICU.
- Nasogastric (NG) tube. A small, flexible tube that keeps the stomach drained of acid and gas bubbles that may build up during surgery.
- Urinary catheter. A small, flexible tube that allows urine to drain out of the bladder and accurately measures how much urine the body makes, which helps determine how well the heart is functioning. After surgery, the heart will be a little weaker than it was before; the body may start to hold onto fluid, causing swelling and puffiness. Diuretics may be given to help the kidneys remove excess fluids from the body.
- Chest tube. A drainage tube may be inserted to keep the chest free of blood that would otherwise accumulate after the incision is closed. Bleeding may occur for several hours or even a few days after surgery.
- Heart monitor. A machine that constantly displays a picture of your child's heart rhythm and monitors heart rate, arterial blood pressure and other values.
Your child may need other equipment, not mentioned here, to provide support while in the ICU or afterwards. The hospital staff will explain all of the necessary equipment to you.
Your child will be kept as comfortable as possible with several different medications; some of which relieve pain and some of which relieve anxiety. The staff may also ask for your input as to how best to soothe and comfort your child.
After discharge from the ICU, your child will recuperate on another hospital unit for a few days before going home. You will learn how to care for your child at home before your child is discharged. Your child may need to take medications for a while and these will be explained to you. The staff will provide instructions regarding medications, activity limitations and follow-up appointments before your child is discharged.
How do I care for my child at home following an ASD repair?
Most children feel comfortable when they go home and have a fair tolerance for activity. Your child may become tired quicker than before the repair but usually will be allowed to play with supervision, while avoiding blows to the chest that might cause injury to the incision or breastbone. Within a few weeks, your child should be fully recovered and able to participate in normal activity.
Pain medications, such as acetaminophen or ibuprofen, may be recommended to keep your child comfortable at home. Your child's physician will discuss pain control before your child is discharged from the hospital.
What is the long-term outlook for my child after ASD repair?
The majority of children who have had an atrial septal defect repair will live healthy lives. Your child's cardiologist may recommend that your child take antibiotics to prevent bacterial endocarditis for a specific time period after discharge from the hospital.
Outcomes also depend on the type of ASD, as well as how early in life the ASD was diagnosed and whether or not it was repaired. With early diagnosis and repair of an ASD, the outcome is generally excellent and minimal follow-up is necessary. When an ASD is diagnosed later in life, if complications occur after surgical closure or the ASD is never repaired, the outlook may be worse than normal. There is a risk of developing pulmonary hypertension (high blood pressure in the blood vessels of the lungs) or Eisenmenger's syndrome. These individuals should receive follow-up care at a center that specializes in congenital heart disease.
Consult your child's physician regarding the specific outlook for your child.
Heart Anatomy Illustration
Atrial Septal Defect Illustration
Meet the Providers Who Treat Atrial Septal Defect (ASD)
Nick's Story
When Nick Cornelius passed his pediatrician's two-year-old well-child check-up with flying colors, his parents were thrilled. Probably even more thrilled than typical first-time toddler parents, because Nick's life up to that point had been anything but typical.
Departments that Treat Atrial Septal Defect (ASD)

Cardiology
The pediatric heart experts at Children's National Hospital in Washington, D.C., provide advanced cardiology care for unborn babies, children and young adults with heart conditions. Learn more about this program.

Pediatric Cardiac Surgery
Children's National is ranked among the nation’s top pediatric heart surgeons, and our team offers advanced care and proven results. Learn more about the procedures available for pediatric cardiac disease and congenital heart defects.

Cardiac Catheterization
We perform hundreds of catheterization procedures every year. We treat children with the most complex heart, blood vessel, and valve conditions. We have one of the highest success rates for cardiac catheterization procedures. Learn more about Cardiac Catheterization.

The Zickler Family Prenatal Pediatrics Institute
The Zickler Family Prenatal Pediatrics Institute at Children's National Hospital in Washington, D.C., provides specialized care for babies during pregnancy, delivery and after birth.

Heart and Lung Center
Our expert pediatric heart team, including more than 40 subspecialties, offer advanced heart care and excellent outcomes for thousands of children every year.
Prenatal Cardiology Program
Children diagnosed with heart conditions before they are born receive comprehensive, expert care from our fetal cardiology specialists. Learn more about our Prenatal Cardiology Program.
Atrioventricular Septal Defects Surgical Outcomes
Learn about some of the lifesaving surgeries our pediatric heart experts perform each year at Children's National. Find outcomes data here.

Help Kids and Make a Difference
Invest in future cures for some of life's most devastating diseases. Give today to help more children grow up stronger.








