Condition
Ventricular Septal Defect (VSD)
What You Need to Know
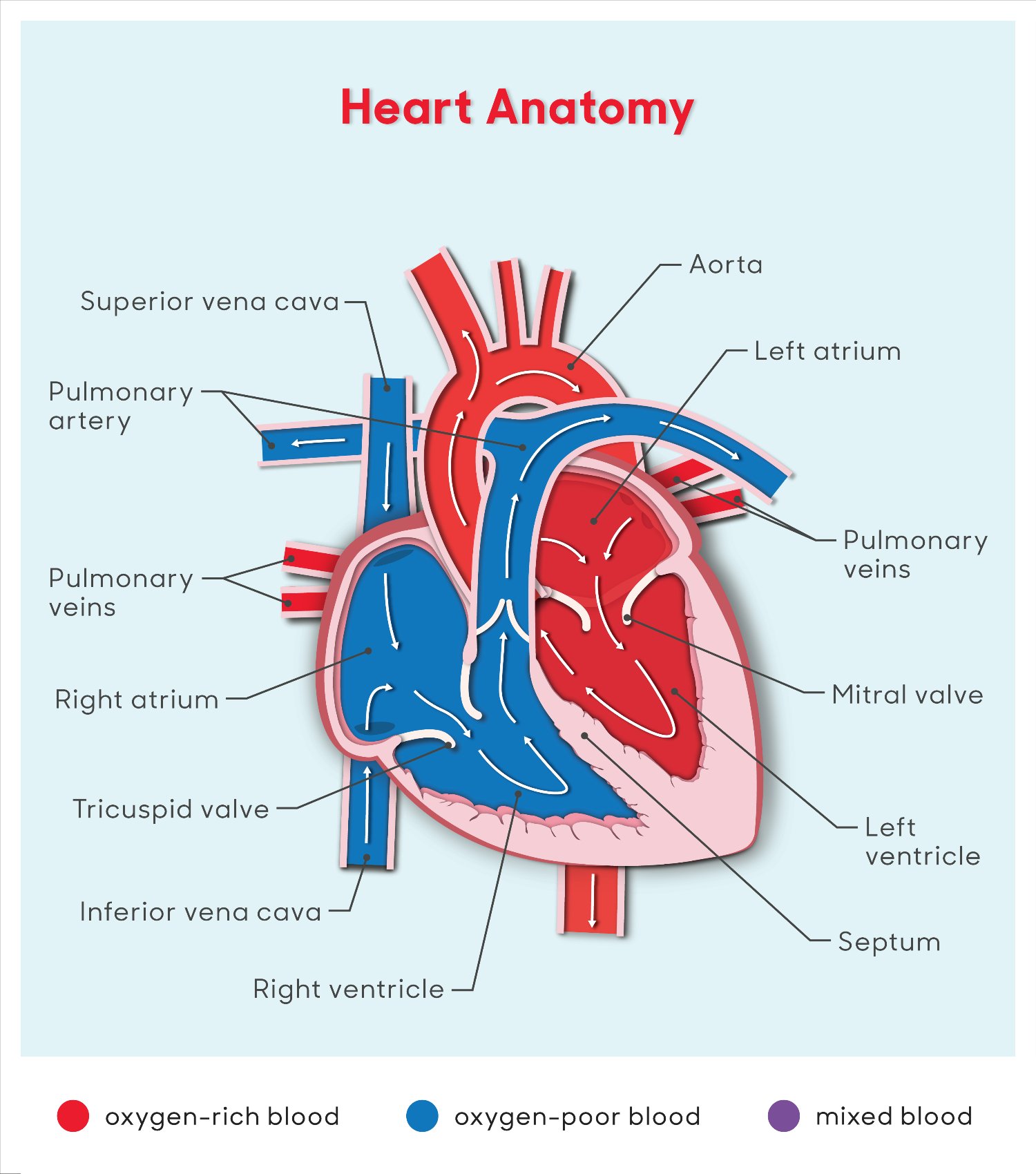
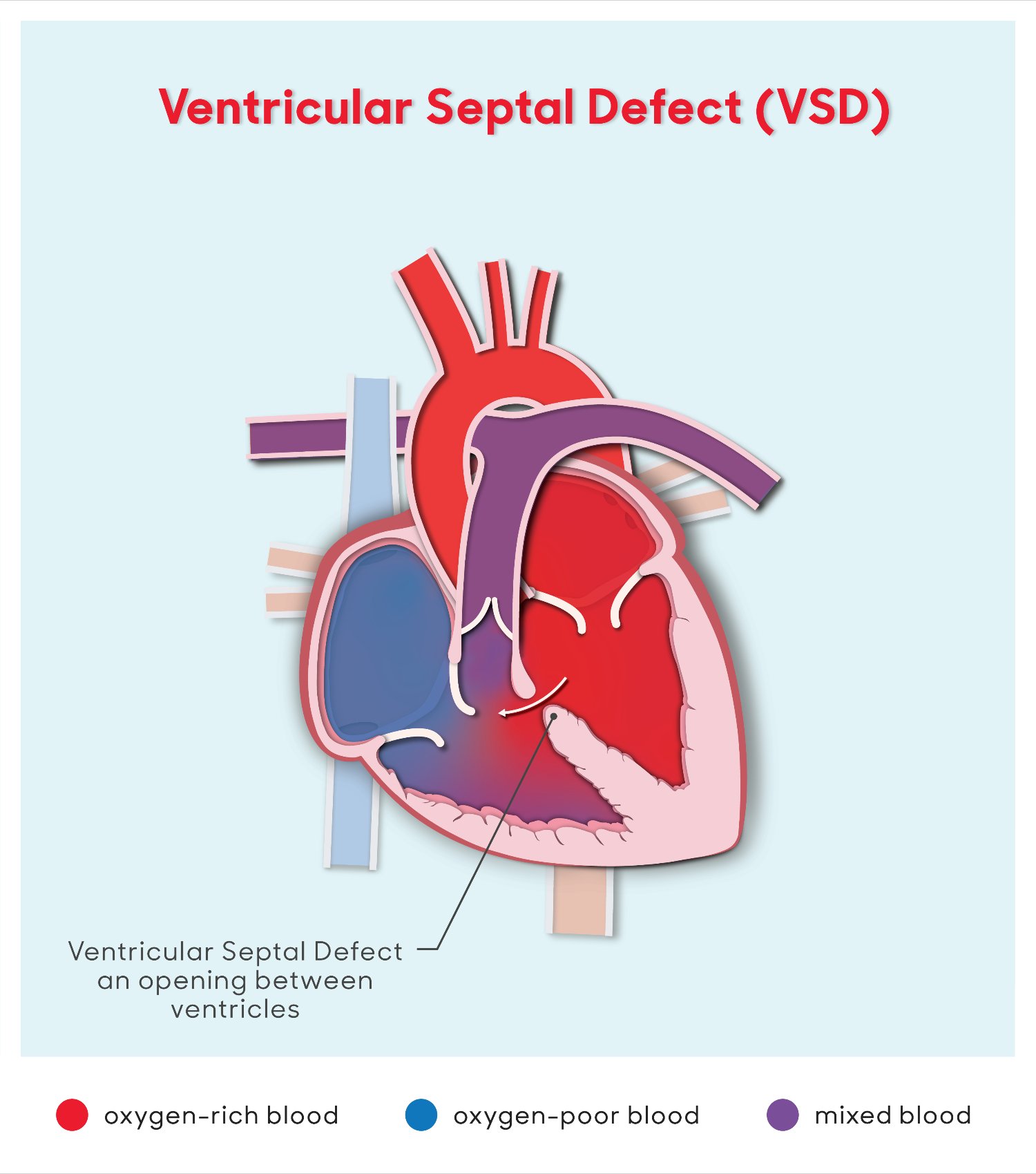
A VSD is an opening in the dividing wall between the two lower chambers of the heart.
Key Symptoms
The most common symptoms of a VSD are:
- Tiredness
- Trouble breathing
- Pale skin
- Rapid heart rate
Diagnosis
Doctors typically diagnose a VSD by:
- Chest X-ray
- Electrocardiogram
- Echocardiogram
Treatment
Treatment may include:
- Medicine
- Surgery
- Cardiac catheterization

Schedule an Appointment
Our pediatric specialists provide personalized care for your child’s physical, mental and emotional health needs. Meet the providers who treat ventricular septal defect and schedule an appointment today.
Frequently Asked Questions
What is a ventricular septal defect?
What causes a VSD in children?
What are the symptoms of a VSD in children?
How is a VSD diagnosed in children?
How is a VSD treated in children?
What are possible complications of a VSD in children?
How can I help my child live with a VSD?
When should I call my child's healthcare provider?
Heart Anatomy Illustration
Ventricular Septal Defect Illustration
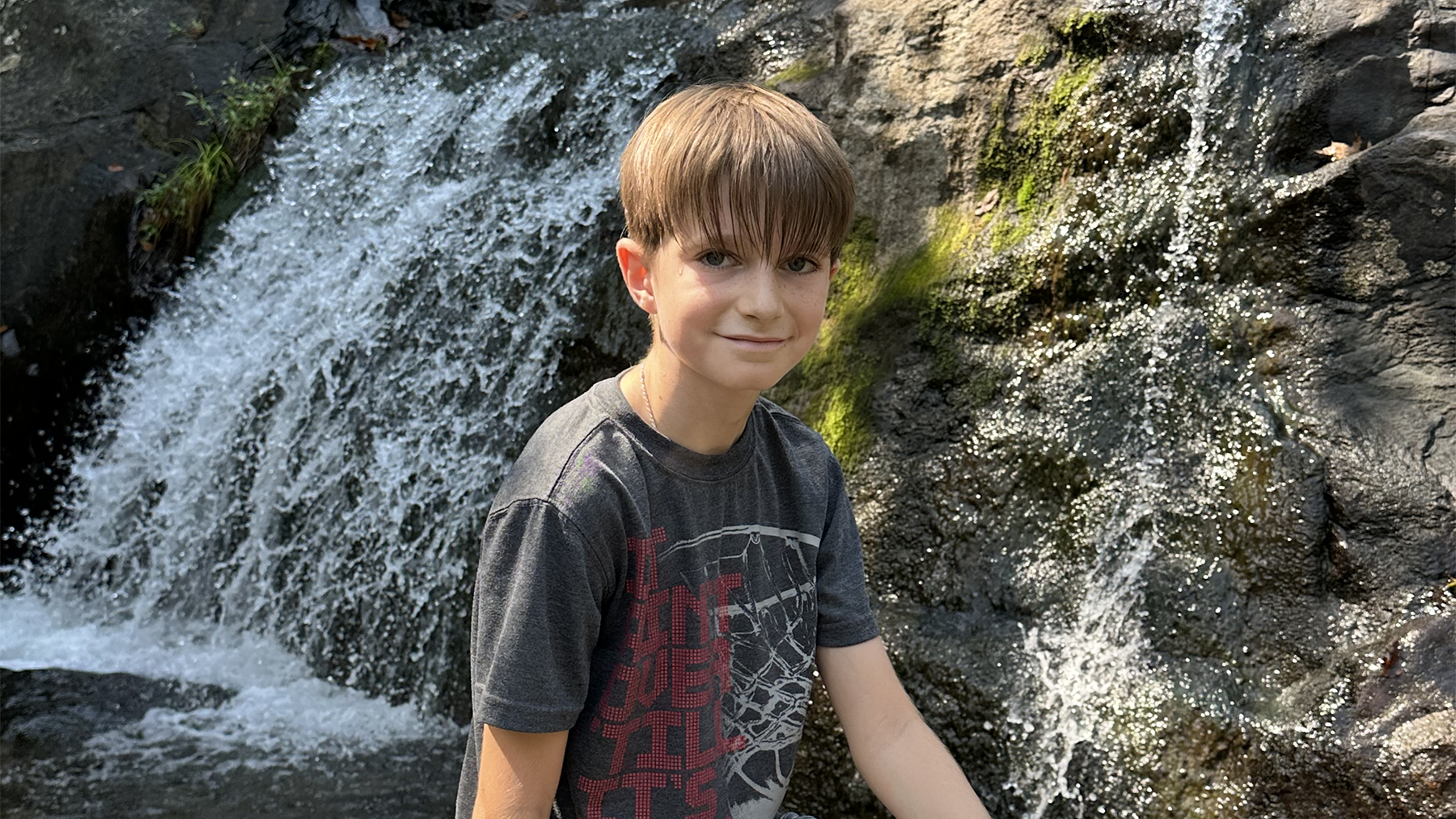
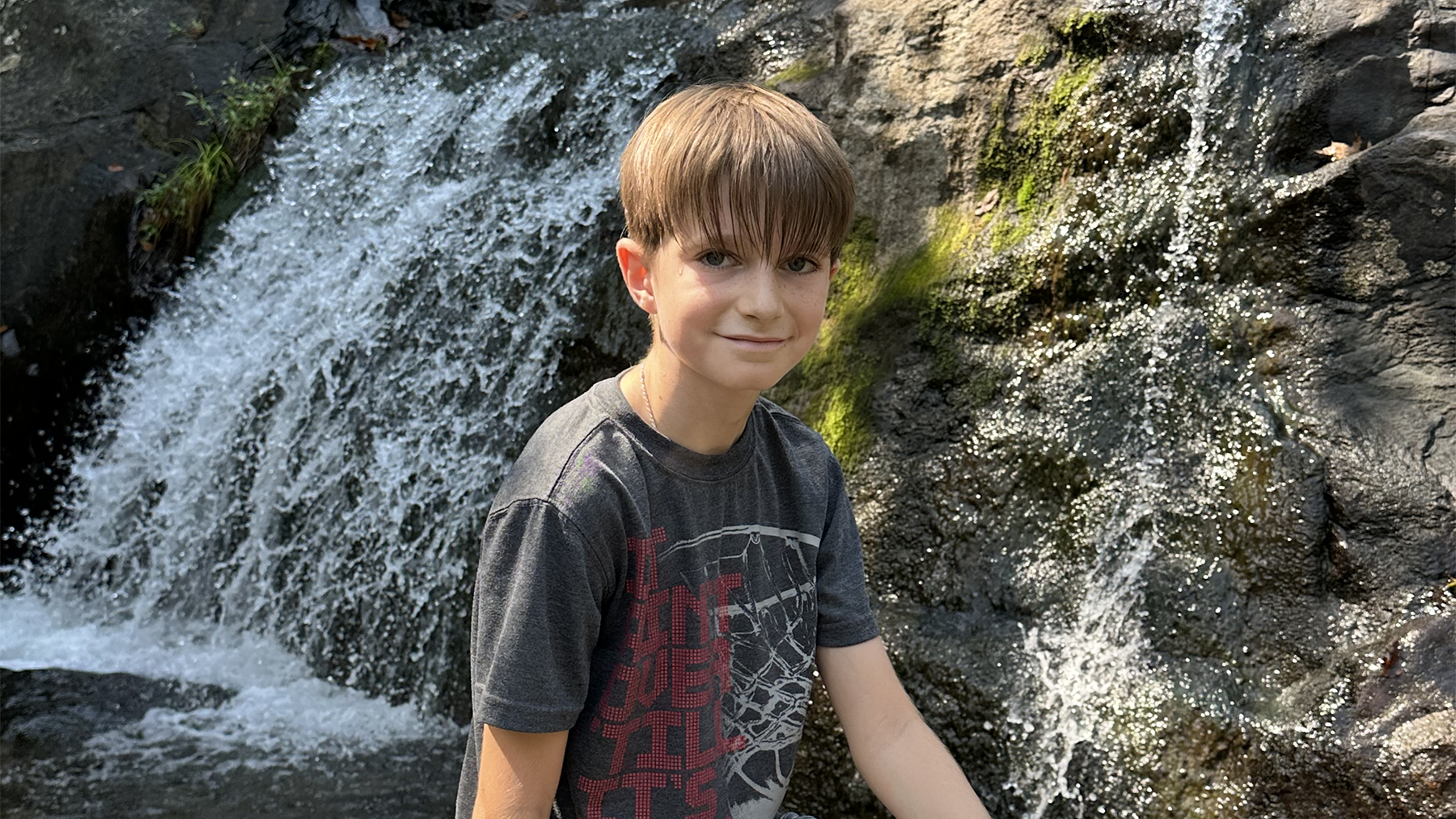
NEWs - Good Morning America
Historic Partial Heart Transplant Replaces Pre-Teen’s Artificial Valve with a Living One
Preston is the first child to have his artificial heart valve replaced with a living valve from a donated heart, thanks to a groundbreaking partial heart transplant performed by our cardiac team.

Cardiac Surgery Outcomes Data
Learn about some of the lifesaving surgeries our pediatric heart experts perform each year at Children's National. Find data about the number of operations, how long children stay in the hospital after surgery (length of stay), and how well they recover after surgery (outcomes).
Departments that Treat Ventricular Septal Defect (VSD)

Cardiac Imaging
We have expertise in the full spectrum of cardiac imaging, including transesophageal, prenatal, 3-D, intracardiac, and stress echocardiography and cardiac MRI.

Help Kids and Make a Difference
Invest in future cures to help children have brighter futures.













