Condition
Pediatric Pulmonary Atresia
What You Need to Know
Pulmonary atresia is an abnormal development of the pulmonary valve.
Key Symptoms
Diagnosis
Treatment
Schedule an Appointment
Our pediatric specialists provide personalized care for your child’s physical, mental and emotional health needs. Meet our providers and schedule an appointment today.
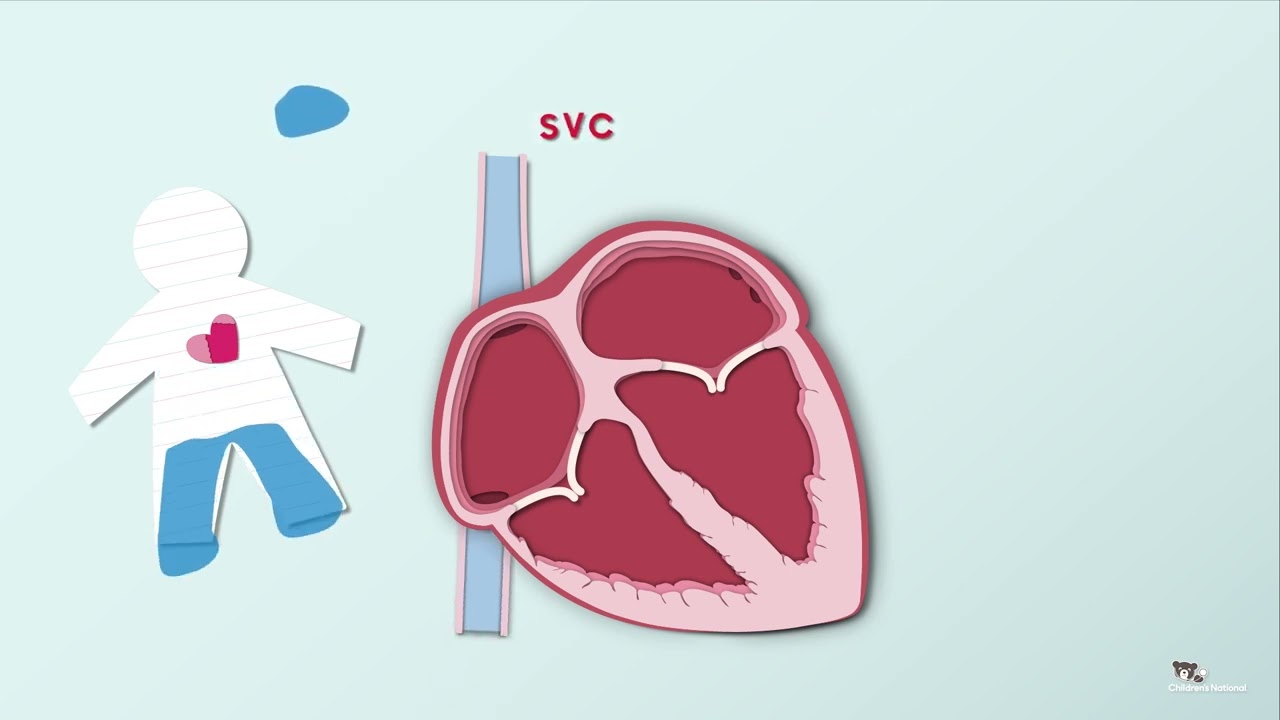
Anatomy of the Heart
This animation presents the anatomy of the heart in detail. Learn about the organ's various parts and the roles that they play.
Frequently Asked Questions
What is pulmonary atresia?
What is pulmonary atresia?
Pulmonary atresia (PA) is a heart defect. It happens when the baby's heart doesn’t form as it should in the uterus. This can happen during the first 8 weeks of pregnancy.
PA is a problem with the opening of the pulmonary valve. This valve connects the right ventricle and the main pulmonary artery. This artery carries blood to the lungs. With PA, blood can’t flow to the lungs.
Since blood can’t flow from the right ventricle to the pulmonary artery, it takes other routes. The normal opening (foramen ovale) between the right and left upper chambers (atria) of the baby's heart normally closes soon after birth. In a newborn with PA, it stays open to let oxygen-poor (blue) blood flow from the right atrium to the left atrium to mix with the oxygen-rich (red) blood returning from the lungs. This mixture of oxygen-poor and oxygen-rich blood is then pumped by the left ventricle out to the body.
In addition, a newborn with PA must rely on a temporary connection (called ductus arteriosus) between the aorta and the pulmonary artery. The ductus arteriosus is part of normal blood flow for a baby in the uterus. But it closes soon after birth. While it is open, some of the mixed blood pumped by the left ventricle flows to the lungs through the patent ductus (PDA) and picks up oxygen. When a child has PA, and the ductus arteriosus closes. No blood reaches the lungs to get oxygen.
Because the blood doesn't get enough oxygen, every cell in the baby's body gets less oxygen. A newborn baby with PA can’t live long without treatment. In some cases, the valve between the right atrium and right ventricle (tricuspid valve) or the right ventricle may be underdeveloped with severe enlargement of the muscle.
What causes pulmonary atresia in children?
What are the symptoms of pulmonary atresia in children?
Symptoms may happen shortly after birth or later as the ductus arteriosus closes. The most clear symptom is a bluish color of the skin (cyanosis) in a newborn.
These are other common symptoms:
- Fast or troubled breathing
- Trouble feeding
- Weakness and sleepiness
- Pale, cool or moist skin
- Seizures
The symptoms of pulmonary atresia may be caused by other health conditions or heart problems. Make sure your child sees a healthcare provider for a diagnosis.
How is pulmonary atresia diagnosed in children?
Pulmonary atresia may be found during a routine ultrasound in pregnancy.
At birth, the healthcare providers and nurses will examine your baby. They will listen to your baby's heart and lungs with a stethoscope and note any signs of a heart defect.
Testing for heart defects varies by the child's age, condition and other things. Some tests that may be done include:
- Pulse oximetry. This test checks oxygen levels in the blood through a tiny clip or band on the baby's hand or foot. PA causes low oxygen levels.
- Chest X-ray. A chest X-ray shows pictures of the heart and lungs. It may show structural problems that occur with PA.
- Electrocardiogram (ECG). This test records the electrical activity of the heart. It shows abnormal rhythms and heart muscle stress.
- Echocardiogram (echo). Echo uses sound waves to record a moving picture of the heart and heart valves. This test is the best test to diagnose pulmonary atresia.
- Cardiac catheterization (heart cath). The baby is sedated with medicine. Then a thin, flexible tube (catheter) is put into a blood vessel in the groin and guided to the heart. A heart cath gives very detailed information about the heart. This includes blood pressure and oxygen measurements in the chambers of the heart, as well as the pulmonary artery and aorta. Contrast dye is also injected to better see the structures in the heart.
What is the treatment for pulmonary atresia in children?
A pediatric cardiologist will treat your baby. This healthcare provider has special training to treat heart problems in children. Your baby will most likely be in the intensive care unit (ICU). At first, your baby may be put on oxygen, and possibly on a machine (ventilator), to help with breathing. Your child may get IV medicines to help their heart and lungs work better.
The below treatments allow time for the oxygen levels in your baby's heart to even out while other repairs are planned:
- An IV medicine called prostaglandin E1 is often given to keep the ductus arteriosus from closing. This lets blood get to the lungs for oxygen.
- A cardiac catheterization may be done to diagnose the defect. In some cases, the pulmonary valve may be able to be opened with catheterization to prevent the need for open heart surgery. This is only an option if the tricuspid valve and the right ventricle are normal size. A procedure can also be done to open or keep open the ductus arteriosus.
Surgical repair
Your child will need surgery to improve blood flow to the lungs. The type of surgery your child has will depend on whether the tricuspid valve or right ventricle can send enough blood to the lungs. Usually, the surgeon will do a series of surgeries to reroute the blood flow to allow oxygen-poor blood to reach the lungs and pick up oxygen. The first surgery may be done shortly after birth. The final surgery is done when the child is a few years old.
What are possible complications of pulmonary atresia in children?
Without surgery, the heart can’t pump oxygenated blood to the body and can’t support life. Surgery can be very successful in those with normal sized tricuspid valves and right ventricles.
As your child grows, they may need to limit physical activity. Your child may also have developmental delays. They may need therapy and special help.
Living with pulmonary atresia
After the surgical repair and time for recovery in the hospital, your baby will be able to go home. Your child's healthcare provider may advise pain medicines such as acetaminophen or ibuprofen to keep your baby comfortable. Your child's heart care team will talk about pain control before your child goes home.
The nursing staff will show you how to give any special treatments at home, if needed. Or you may need a home health agency to help. Your child will likely need special formula and supplemental feedings to get enough nutrition.
You may get other instructions from your child's pediatric cardiologist and the hospital staff.
The outlook varies from child to child. Be sure to get regular follow-up care at a center offering pediatric congenital heart care. Your child likely will need more surgery.
After each surgery, your pediatric cardiologist will follow your baby’s recovery. They will make changes to medicines, help you with feeding problems, measure oxygen levels, and determine when and if it is time for the next surgery.
Your child may need to be on long-term antibiotics or take antibiotics before dental or other procedures. Your healthcare provider can tell you if this is needed.
It is important that your child get all recommended vaccines. Talk with your healthcare provider about this.
During your child's life, pregnancy and nonheart surgeries may be very risky. They require careful evaluation and discussion with a cardiologist.
Your child will need regular follow-up care at a center offering pediatric or adult congenital heart care for the rest of their life.
What postoperative care can I expect for my child?
After surgery, infants will return to the ICU to be closely monitored during recovery.
While your child is in the ICU, special equipment will be used to help him or her recover, and may include the following:
- Ventilator. A machine that helps your child breathe while he or she is under anesthesia during the operation. A small, plastic tube is guided into the windpipe and attached to the ventilator, which breathes for your child while he or she is too sleepy to breathe effectively on his or her own. After a pulmonary atresia, children will benefit from remaining on the ventilator overnight or even longer so they can rest.
- Intravenous (IV) catheters. Small, plastic tubes inserted through the skin into blood vessels to provide IV fluids and important medicines that help your child recover from the operation.
- Arterial line. A specialized IV placed in the wrist or other area of the body where a pulse can be felt, that measures blood pressure continuously during surgery and while your child is in the ICU.
- Nasogastric (NG) tube. A small, flexible tube that keeps the stomach drained of acid and gas bubbles that may build up during surgery.
- Urinary catheter. A small, flexible tube that allows urine to drain out of the bladder and accurately measures how much urine the body makes, which helps determine how well the heart is functioning. After surgery, the heart will be a little weaker than it was before, and, therefore, the body may start to hold onto fluid, causing swelling and puffiness. Diuretics may be given to help the kidneys remove excess fluid from the body.
- Chest tube. A drainage tube may be inserted to keep the chest free of blood that would otherwise accumulate after the incision is closed. Bleeding may occur for several hours, or even a few days after surgery.
- Heart monitor. A machine that constantly displays a picture of your child's heart rhythm, and monitors heart rate, arterial blood pressure, and other values.
Your child may need other equipment not mentioned here to provide support while in the ICU, or afterwards. The hospital staff will explain all of the necessary equipment to you.
Your child will be kept as comfortable as possible with several different medications; some relieve pain, and some relieve anxiety. The staff will also ask for your input on how best to soothe and comfort your child.
After discharge from the ICU, your child will recuperate in another hospital unit before going home. You will learn how to care for your child at home before your child is discharged. Your child may need to take medications for a while. The staff will give you written instructions regarding medications, activity limitations, and follow-up appointments before your child is discharged.
Infants who spent a lot of time on a ventilator, or who were fairly ill while in the ICU, may have trouble feeding initially. These babies may have an oral aversion; they might equate something placed in the mouth, such as a pacifier or bottle, with a less pleasant sensation, such as being on the ventilator. Some infants are just tired, and need to build their strength up before they will be able to learn to bottle-feed. Strategies used to help infants with nutrition include the following:
- High-calorie formula or breast milk. Special nutritional supplements may be added to formula or pumped breast milk that increase the number of calories in each ounce, thereby allowing your baby to drink less and still consume enough calories to grow properly.
- Supplemental tube feedings. Feedings given through a small, flexible tube that passes through the nose, down the esophagus, and into the stomach, that can either supplement or take the place of bottle feedings. Infants who can drink part of their bottle, but not all, may be fed the remainder through the feeding tube. Infants who are too tired to bottle feed at all may receive their formula or breast milk through the feeding tube alone.
How can I care for my child at home following a pulmonary atresia surgical repair?
Pain medications, such as acetaminophen or ibuprofen, may be recommended to keep your child comfortable. Your child's physician will discuss pain control before your child is discharged from the hospital.
If any special treatments are to be given at home, the nursing staff will ensure that you are able to provide them, or a home health agency may assist you.
You may receive additional instructions from your child's physicians and the hospital staff.
What is the long-term outlook for children after pulmonary atresia surgical repair?
The outlook varies from child to child. Follow-up care at a center offering pediatric congenital cardiac care should be carried out regularly. It is not unexpected for multiple reoperations to be performed to replace conduits or revise a palliation.
After each operation, your infant will need to be followed by a pediatric cardiologist, who will make adjustments to medications, assist you with feeding problems, measure oxygen levels and determine when it is time for the next operation.
There is significant risk for progressive development of complications, such as heart failure, dysrhythmias and protein-losing enteropathy (liver congestion).
Pregnancy and other noncardiac surgeries pose major risks and require careful evaluation and discussion with a congenital cardiologist.
Regular follow-up care at a center offering pediatric or adult congenital cardiac care should continue throughout the individual’s lifespan.
Consult your child's physician regarding the specific outlook for your child.
Meet the Providers Who Treat Pulmonary Atresia
Zach's Story
Zachary Blumenfeld is so thankful for the Children's National Hospital physicians who saved his life. Now, he wants to spread miracles around the world.
Departments that Treat Pulmonary Atresia

Cardiac Imaging
We have expertise in the full spectrum of cardiac imaging, including transesophageal, prenatal, 3-D, intracardiac, and stress echocardiography and cardiac MRI.

Cardiology
The pediatric heart experts at Children's National Hospital in Washington, D.C., provide advanced cardiology care for unborn babies, children and young adults with heart conditions. Learn more about this program.

Pediatric Cardiac Surgery
Children's National is ranked among the nation’s top pediatric heart surgeons, and our team offers advanced care and proven results. Learn more about the procedures available for pediatric cardiac disease and congenital heart defects.

Cardiac Catheterization
We perform hundreds of catheterization procedures every year. We treat children with the most complex heart, blood vessel, and valve conditions. We have one of the highest success rates for cardiac catheterization procedures. Learn more about Cardiac Catheterization.

The Zickler Family Prenatal Pediatrics Institute
The Zickler Family Prenatal Pediatrics Institute at Children's National Hospital in Washington, D.C., provides specialized care for babies during pregnancy, delivery and after birth.

Heart and Lung Center
Our expert pediatric heart team, including more than 40 subspecialties, offer advanced heart care and excellent outcomes for thousands of children every year.
Prenatal Cardiology Program
Children diagnosed with heart conditions before they are born receive comprehensive, expert care from our fetal cardiology specialists. Learn more about our Prenatal Cardiology Program.

Help Kids and Make a Difference
Invest in future cures for some of life's most devastating diseases. Give today to help more children grow up stronger.