Condition
Viral Rashes
What You Need to Know
A viral rash (also known as an exanthem) is an eruptive skin rash that is often related to a viral infection.
Key Symptoms
The most common symptoms of viral rashes include:
- Itchy, red or irritated skin (rash)
- Flat or raised lesions on the skin
- Fever
Diagnosis
Doctors typically diagnose viral rashes by:
- Physical examination
Treatment
- The treatment depends on the type of rash and symptoms the child is experiencing
Schedule an Appointment
Our pediatric specialists provide personalized care for your child’s physical, mental and emotional health needs. Meet our providers and schedule an appointment today.
Types of Viral Rashes
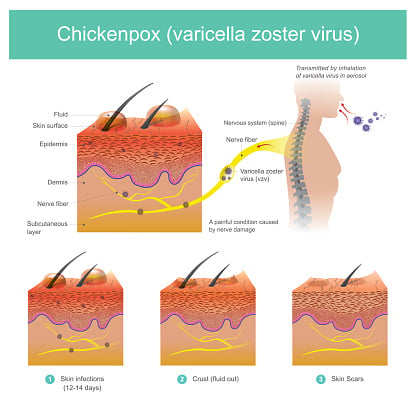
Chickenpox
 What is chickenpox?
What is chickenpox?
Chickenpox is a highly infectious disease, usually associated with childhood. By adulthood, more than 95 percent of Americans have had chickenpox.
The disease is caused by the varicella-zoster virus (VZV), a form of the herpes virus. Transmission occurs from person-to-person by direct contact or through the air.
Chickenpox most commonly occurs in children between the ages of 5 and 9. In the US, in areas with a large number of children in daycare settings, chicken pox in children between the ages of 1 and 4 is common.
What is the chickenpox vaccine?
Since 1995, a chickenpox vaccine has been available for children 12 months of age and older. Adolescents and adults who have never had chickenpox can also get the vaccine. The vaccine has proven very effective in preventing severe chickenpox.
The Center for Disease Control & Prevention’s Advisory Committee on Immunization Practices, the American Academy of Pediatrics, and the American Academy of Family Physicians recommend that all children be vaccinated with the chickenpox vaccine between 12 and 18 months of age.
A booster vaccination is recommended again between 11 and 12 years of age. Many schools now require vaccination prior to entry into preschool or public schools.
What are the symptoms of chickenpox?
Symptoms are usually mild among children, but may be life threatening to infants, adults, and people with impaired immune systems.
The following are the most common symptoms of chickenpox. However, each child may experience symptoms differently. Symptoms may include:
- Fatigue and irritability one to two days before the rash begins
- Itchy rash on the trunk, face, under the armpits, on the upper arms and legs, and inside the mouth
- Fever
- Feeling ill
- Decreased appetite
- Muscle and/or joint pain
- Cough or runny nose
The symptoms of chickenpox may resemble other skin problems or medical conditions. Always consult a physician for a diagnosis.
How is chickenpox spread?
Once infected, chickenpox may take 10 to 21 days to develop. Chickenpox is contagious for one to two days before the appearance of the rash and until the blisters have dried and become scabs, which usually happens within 4 to 5 days of the onset of the rash.
Children should stay home and away from other children until all of the blisters have scabbed over. Family members who have never had chickenpox have a 90 percent chance of becoming infected when another family member in the household is infected.
How is chickenpox diagnosed?
Chickenpox is usually diagnosed based on a complete medical history and physical examination of the child. The rash of chickenpox is unique, and usually a diagnosis can be made from a physical examination.
What is the treatment for chickenpox?
The specific treatment for chickenpox will be determined based on:
- The child's age, overall health, and medical history extent of the condition
- The child's tolerance for specific medications, procedures, or therapies
- Expectations for the course of the condition child or parent's opinion or preference
Aspirin and the Risk of Reye Syndrome in Children
Do not give aspirin to a child without first contacting the child's physician. Aspirin has been associated with Reye syndrome, a potentially serious or deadly disorder in children. Pediatricians and other healthcare providers recommend that aspirin (or any medication that contains aspirin) not be used to treat any viral illnesses in children.
The treatment for chickenpox may include:
- Acetaminophen for fever (DO NOT GIVE ASPIRIN)
- Antibiotics for treating bacterial infections
- Calamine lotion (to relieve itching)
- Antiviral drugs (for severe cases)
- Rest
- Increased fluid intake (to prevent dehydration)
- Cool baths with baking soda or Aveeno (to relieve itching)
Children should not scratch the blisters, as this can lead to secondary bacterial infections. Keep the child's fingernails short to decrease the likelihood of scratching.
What is immunity from chickenpox?
Most individuals who have had chickenpox will be immune to the disease for the rest of their lives. However, the virus remains dormant in nerve tissue and may reactivate, resulting in herpes zoster (shingles) later in life.
Occasionally a secondary case of chickenpox does occur. Blood tests can confirm immunity to chickenpox in people who are unsure if they have had the disease.
What complications are commonly associated with chickenpox?
Complications can occur from chickenpox. Those most susceptible to severe cases of chickenpox are infants, adults, pregnant women (unborn babies may be infected if the mother has not had chickenpox prior to pregnancy), and people with impaired immune systems. Complications may include:
- Secondary bacterial infections
- Pneumonia
- Encephalitis (inflammation of the brain)
- Cerebellar ataxia (defective muscular coordination)
- Transverse myelitis (inflammation along the spinal cord)
- Reye syndrome (a serious condition which may affect all major systems or organs)
- Death
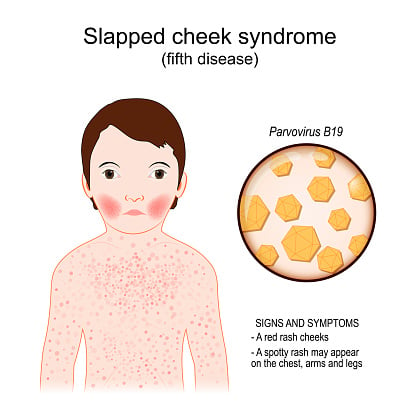
Fifth Disease
 What is fifth disease?
What is fifth disease?
Fifth disease is a viral illness that causes a rash (exanthem). Fifth disease is also called erythema infectiosum. And it's known as "slapped cheek" disease. This is because the rash can cause a child's cheeks to become very red. Fifth disease is spread from one child to another through direct contact with fluid from the nose and throat. It can also be spread through contact with infected blood. It is somewhat contagious.
What causes fifth disease?
Fifth disease is caused by human parvovirus B19. It occurs most often in the winter and spring.
Which children are at risk for fifth disease?
It is most common in young, school-age children. Children often get it at school or other places where children gather. Adults can get fifth disease, too, but most infections are in children.
What are the symptoms of fifth disease?
Symptoms usually show up 4 to 14 days after a child is exposed to the disease. About 4 in 5 infected children have very mild symptoms for about a week before getting the rash. About 1 in 5 will have no symptoms at all before the rash appears. Children are most contagious before the rash occurs, before they know they have the disease.
Early symptoms are usually very mild. These may include:
- Low fever
- Headache
- Runny nose
- Sore throat
- Itching
- Nausea or vomiting
- Diarrhea
A rash is usually the main symptom of fifth disease. The rash:
- Starts on the cheeks and is bright red
- Spreads to the trunk, arms, and legs, and lasts 2 to 4 days. It often has a "lacey" appearance.
- May come back when the child is exposed to sunlight, heat or cold, or injury to the skin. This may continue for several days.
The symptoms of fifth disease can be like other health conditions. Make sure your child sees their healthcare provider for a diagnosis.
Warning
Pregnant women who have been exposed to fifth disease need to seek immediate medical attention.
Fifth disease is usually a mild illness. However, parvovirus B19 infection can cause an acute severe anemia in persons with sickle-cell disease or immune deficiencies. Also, there is a small risk of fetal death if fifth disease is acquired during pregnancy.
The symptoms of fifth disease may resemble other conditions or medical problems, so consult a physician for proper diagnosis.
How is fifth disease diagnosed?
The healthcare provider will ask about your child's symptoms and health history. They will give your child a physical exam. The physical exam will include inspecting the rash. The rash is unique to fifth disease and may be enough to diagnose your child. In some cases, your child may also have blood tests.
What is the treatment for fifth disease?
Treatment will depend on your child's symptoms, age, and general health. It will also depend on how severe the condition is. The illness is caused by a virus. Antibiotics won't help your child.
The goal of treatment is to help ease symptoms. Treatment may include:
- Having your child drink plenty of fluids
- Giving acetaminophen or ibuprofen for fever and discomfort
- Giving an antihistamine medicine for itching
Talk with your child's healthcare providers about the risks, benefits and possible side effects of all medicines. Don't give ibuprofen to a child younger than 6 months old unless your healthcare provider tells you to. Don't give aspirin to children. Aspirin can cause a serious health condition called Reye syndrome.
Aspirin and the Risk of Reye Syndrome in Children
Do not give aspirin to a child without first contacting the child's physician. Aspirin has been associated with Reye syndrome, a potentially serious or deadly disorder in children. Pediatricians and other healthcare providers recommend that aspirin (or any medication that contains aspirin) not be used to treat any viral illnesses in children.
What are possible complications of fifth disease in a child?
Fifth disease is usually a mild illness. In some cases, it may cause acute severe anemia in a child with sickle cell disease or a weak immune system. In a pregnant woman with fifth disease, there is a small risk of death of the baby in the womb.
How can I help prevent fifth disease in my child?
The best ways to keep fifth disease from spreading include:
- Washing hands well with soap and warm water
- Covering the mouth and nose when coughing or sneezing
When should I call my child's healthcare provider?
Call the healthcare provider if your child has:
- Symptoms that don't get better, or get worse
- New symptoms
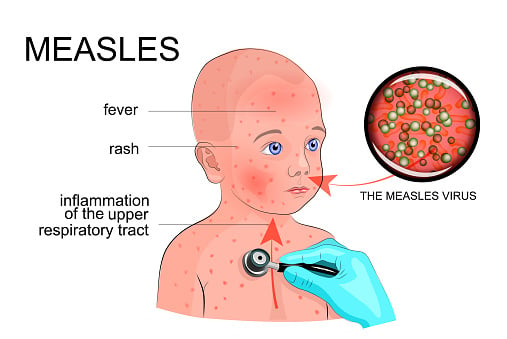
Measles (or Rubeola)
- Measles is a highly contagious disease that usually consists of a rash, fever and cough.
- It is spread from one child to another through direct contact with discharge from the nose and throat, or via airborne droplets from an infected child.
- Getting vaccinated can protect your family from the measles.
Learn more about measles and read our frequently asked questions for patients and families in English or Spanish.
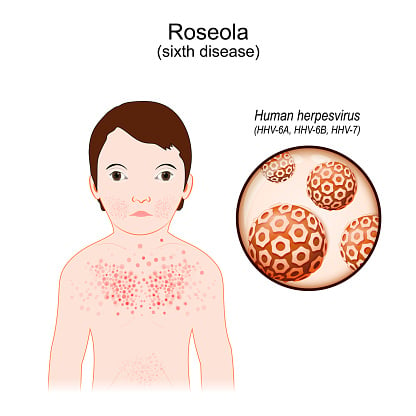
Roseola
 What is roseola?
What is roseola?
Roseola is a contagious viral illness that is marked by a high fever and a rash that develops as the fever decreases.
What causes roseola?
Roseola is likely caused by more than one virus, but the most common cause is the human herpesvirus 6 (HHV-6). Roseola occurs mostly in children under the age of 3, and occurs more often in the spring and fall.
What are the symptoms of roseola?
It can take between 5 and 15 days for a child to develop symptoms of roseola after being exposed to the disease. Children are most contagious during the period of high fever, before the rash occurs.
The following are the most common symptoms of roseola. However, each child may experience symptoms differently.
- High fever that starts abruptly
- Fever (may last three to four days)
- Irritability
- Swelling of the eyelids
- Rash (as the fever decreases, a pink rash, with either flat or raised lesions, starts to appear on the trunk and then spreads to the face, arms, and legs.)
What are the complications of roseola?
The most serious complication of roseola is febrile seizures. As the child's temperature rises, there is a chance that the child will have a seizure.
The symptoms of roseola may resemble other skin conditions or medical problems. Always consult a physician for the proper diagnosis.
How is roseola diagnosed?
Roseola is usually diagnosed based on a medical history and physical examination of your child. The rash of roseola that follows a high fever is unique, and often the diagnosis is made simply on physical examination.
Aspirin and the Risk of Reye Syndrome in Children
Do not give aspirin to a child without first contacting the child's physician. Aspirin has been associated with Reye syndrome, a potentially serious or deadly disorder in children. Pediatricians and other healthcare providers recommend that aspirin (or any medication that contains aspirin) not be used to treat any viral illnesses in children.
What is the treatment for roseola?
The specific treatment for roseola will be determined based on:
- The child's age, overall health, and medical history
- Extent of the disease
- The child's tolerance for specific medications, procedures, or therapies
- Expectations for the course of the disease
- Child or parent’s opinion or preference
Since it is a viral infection, there is no cure for roseola. The goal of treatment for roseola is to help decrease the severity of the symptoms. Treatment may include increased fluid intake or acetaminophen for fever (DO NOT GIVE ASPIRIN).
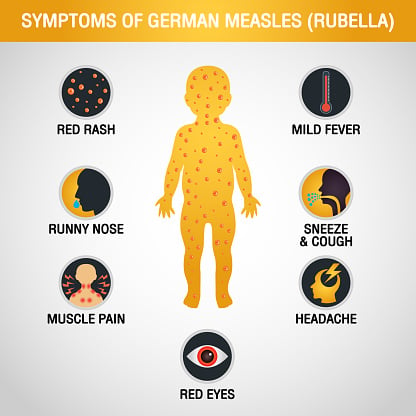
Rubella (German Measles)
 Rubella is a viral illness that causes a mild fever and a skin rash. Rubella is spread through contact with fluid from the nose and throat. Learn more about rubella.
Rubella is a viral illness that causes a mild fever and a skin rash. Rubella is spread through contact with fluid from the nose and throat. Learn more about rubella.
Illustrations of Viral Rashes
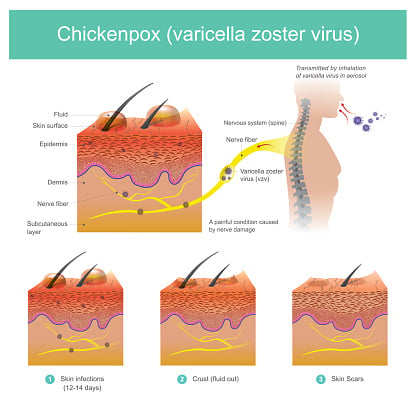
Chickenpox
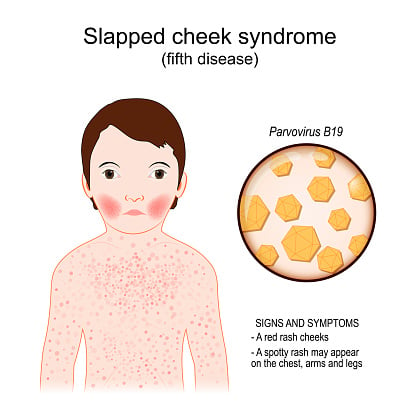
Fifth Disease
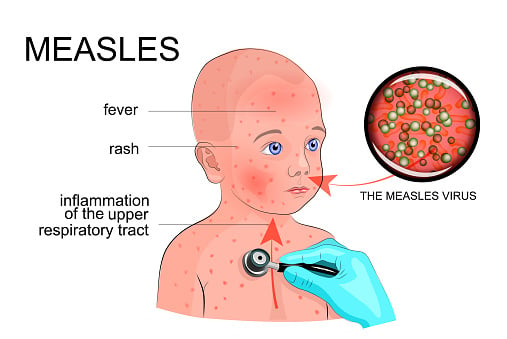
Measles
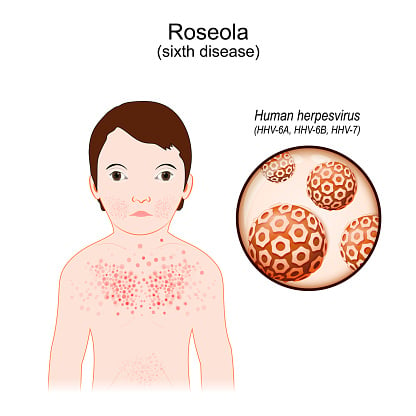
Roseola
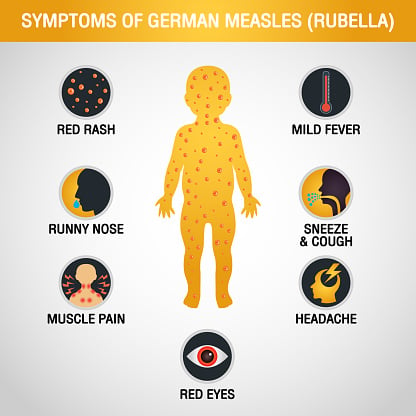
Rubella
Meet the Providers Who Treat Viral Rashes
Departments that Treat Viral Rashes

Infectious Diseases
Our Division of Infectious Diseases is the major referral center for infectious diseases in the Washington, D.C., area, helping thousands of patients each year, and actively promoting prevention through community outreach and education. Learn more about this division.

Dermatology
The Division of Dermatology at Children's National Hospital continues to expand services as more families seek our expertise in the diagnosis and treatment of disorders of the skin, hair and nails. Learn more about our division.

General & Community Pediatrics
Children's National Hospital has the largest pediatric presence in the Washington, D.C., area. Our primary care practices are one way we carry out the mission at Children's National to expand access to quality healthcare and improve health outcomes for children in the community.

Help Kids and Make a Difference
Invest in future cures for some of life's most devastating diseases. Give today to help more children grow up stronger.








