Noah's Story
 After Joshua and Sandra Sweek noticed that their 6-month-old son, Noah, was having breathing problems, they took him to the doctor. There, the baby was diagnosed with suspected asthma. Noah was prescribed what felt like a pharmacy full of medications, Joshua says, including oral drugs, maintenance breathing treatments and a rescue inhaler. But they received little guidance about how to manage Noah’s condition effectively.
After Joshua and Sandra Sweek noticed that their 6-month-old son, Noah, was having breathing problems, they took him to the doctor. There, the baby was diagnosed with suspected asthma. Noah was prescribed what felt like a pharmacy full of medications, Joshua says, including oral drugs, maintenance breathing treatments and a rescue inhaler. But they received little guidance about how to manage Noah’s condition effectively.
“Everyone kept telling us he’d grow out of it, so they never guided us on what to do about it,” Joshua says.
That lack of knowledge resurfaced repeatedly in a slew of negative consequences over the next several years. With no knowledge of triggers for Noah’s asthma symptoms, no education on the best way to administer his medications and no real understanding of asthma in general, the family found themselves in their local hospital’s Emergency Department every two to three months over the next seven years to get treatments for Noah’s asthma flare-ups.
As a bartender with no insurance, Joshua frequently worked overtime to pay the family’s enormous medical bills. Even when Noah seemed well, his parents were on constant alert to make sure their medically fragile child was OK.
“We spent a lot of sleepless nights just watching his chest rise and fall to make sure he was still breathing,” Joshua remembers.
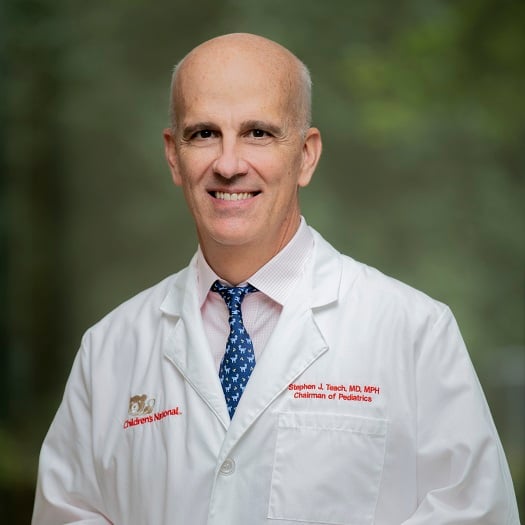
A particularly terrifying event finally prompted change. When Noah was 7, he had an asthma attack more intense than any he’d ever had before. Both of his lungs collapsed, sending him to the intensive care unit at Children’s National Hospital for one week. Never leaving Noah’s side, Joshua was visited by a multitude of care providers, including Stephen J. Teach, M.D., M.P.H., the director and principal investigator for IMPACT DC, the award-winning program that aims to improve asthma care and outcomes for children in the District of Columbia area.
“Noah had all these machines connected to him. It was pretty intense,” Joshua says. “It was a horrible situation, but it was a blessing in disguise because it put us on the path to better understanding his condition.”
Dr. Teach asked to take over Noah’s care and connected the family to IMPACT DC. Joshua and Sandra began receiving teaching through IMPACT DC, catching up on seven years of asthma knowledge. With Dr. Teach’s help, they learned Noah’s triggers include winter weather, cigarette smoke, dust and exposure to damp, cold conditions like getting soaked by rain. The couple also learned more about what Noah goes through when he experiences an asthma flare-up.
“They told us to imagine putting a bag over our heads and trying to breathe or imagine breathing through a coffee straw,” Joshua says.
Now 14 years old and a high school freshman, Noah has an asthma flare-up strong enough to send him to the Emergency Department about once a year—a marked reduction from the four to six times a year in the past. He stays active, wrestling with his 8-year-old brother, playing basketball and swimming.
“It’s all about keeping his asthma under control as best we can and just letting him live his life,” Joshua says. “My hope is that he can live a good, normal life and never let this stop him from doing anything he wants to do.”