Children's National Launches Electronic Health Record Dashboards, Shows Improved Quality and Safety in PICU
Washington, DC –Children’s National Health System has launched real-time, automated electronic health record dashboards in the Pediatric Intensive Care Unit (PICU) that have resulted in significant improvement in quality and safety of care, new research shows.
“We found that having a visible, unit-wide, real-time dashboard improves the dynamic nature of care delivery and increases awareness for potential interventions,” said Brian Jacobs, MD, Vice President, Chief Medical Information Officer and Chief Information Officer, Executive Director, Center for Pediatric Informatics at Children’s National.
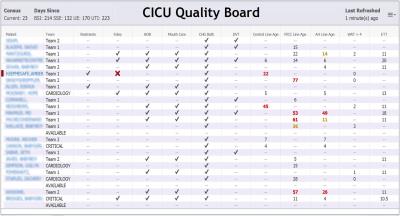
The Children’s National electronic dashboards are HIPAA compliant communications, displayed in publicly restricted areas and for use by parents and staff, containing visual displays of patient names and quality metrics providing checkpoints for nurses and doctors to continually monitor care, with updates every five minutes. This data is pulled directly from the electronic health records.
By using dashboards in the PICU, Children’s National has significantly decreased the number of urinary catheter days and catheter-associated urinary tract infections (CAUTI), one of the most commonly reported hospital-acquired conditions. In addition, the dashboards include a comprehensive list of all medications a patient is given, a process known as medication reconciliation.
“We try to engage patients and families in the process, so they can be part of the care delivery team, not just passive recipients,” Dr. Jacobs said of the electronic dashboard. "In full view, parents can look up, see their child’s name, and know what is and isn’t being done. For instance, if they haven’t had an antiseptic bath, it’s marked red with a big X.”
The dashboards also are important for doctors and nurses, because “they can ask themselves, ‘what can I do today on my shift, right now, to improve safety and quality,” said Dr. Jacobs.
Jacobs and other Children’s National researchers reported about the hospital system’s success in using the automated health record dashboard, in a study entitled, “Effect of a Real-Time Pediatric ICU Safety Bundle Dashboard on Quality Improvement Measures,” published this month in The Joint Commission Journal on Quality and Patient Safety.
Over a period of three months, they found:
- The time from a patient’s admission to the PICU and obtaining treatment consent decreased from 393 to 304 minutes, showing a 49 percent improvement.
- The number of patients with CAUTI decreased from 4.5 events per 1,000 urinary catheter days, to 3.1 events per 1,000 days, a decline from 32 to 19 percent.
- Medication reconciliation accuracy and completion increased from 80 percent to 93 percent.
The study showed that a dashboard with real-time quality and safety information can result in better outcomes than historic approaches such as safety checklists or patient goal sheets. While those processes are often successful, they have limitations in management of critically ill patients, Dr. Jacobs says. “Patient goal sheets are static, and may not be checked for 24 hours. A lot of things can happen in that time,” he said. “On the other hand, electronic health records are instantaneous. This is a dynamic change.”
The study did not find differences in outcomes of patients who had pressure ulcers, or deep vein thrombosis (blood clots that form in veins). Besides the PICU, Children’s National also has installed the dashboards in the cardiac and neonatal units. Eventually, it will be included in the acute care, surgical care, and neurology units.
“My personal goal is that this technology will be present in every one of the 5,800 hospitals in the country,” Dr. Jacobs said. “This is a big paradigm shift in care, and it isn’t something we have to wait for. Why not do it now.”
Contact: Caitlyn Camacho at 202-476-4500.



